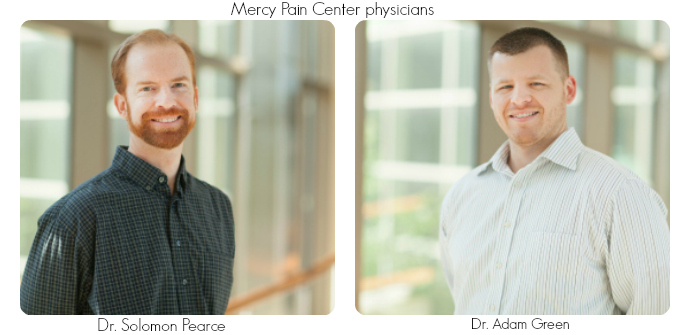
Note from the Mamas: This is a continuation of last week’s interview of Dr. Solomon Pearce of the Mercy Pain Center about managing chronic pain. (Click here to read the first post.)
The stress of parenthood coupled with untreated daily pain can be an overwhelming situation for anyone. That’s why we asked an expert at the Mercy Pain Center to give us some insight about the field of Pain Management as well as the latest advancements in the field and what every patient needs to know before she lets someone treat her pain. We learned a lot from his answers below.
What are the most common mistakes patients make when trying to manage chronic pain? What do you wish more people understood about this field of medicine?
Having the wrong attitude when it comes to any chronic condition is a pivotal mistake. In particular, a number of chronic pain patients fall into the trap of taking a completely passive role in their own condition. They constantly look for others to do something, give them something, make them feel better, but some patients are unwilling to do anything for themselves.
It’s often hard to realize that your pain is your own. Despite the best intentions of others, ultimately it is your responsibility to get better. What this means is  taking an active role in your health. If you have weak muscles, do your physical therapy. If you’re overweight, lose weight. If you have diabetes, keep tight control of your condition. If you use tobacco products, stop. If you have a stressful life, meditate or do yoga or a hundred other things that you can do to get better.
taking an active role in your health. If you have weak muscles, do your physical therapy. If you’re overweight, lose weight. If you have diabetes, keep tight control of your condition. If you use tobacco products, stop. If you have a stressful life, meditate or do yoga or a hundred other things that you can do to get better.
Some of the most difficult things to do are some of the most beneficial. I strongly encourage all my patients to take a hard look at why they might be suffering so much, when someone else with the same physical problem is functioning fine. Often times these patients realize that they have never dealt with past traumas like physical or sexual abuse. Some realize that they hate their job or are really unhappy in their relationship. Once these issues are dealt with, their pain often gets dramatically better.
I wish people understood that healthcare has become a business and that you have to be careful where you shop. There are a lot of unscrupulous people out there selling hope in the form of medication, supplements, surgeries, or the newest device or procedure. All these can have unwanted effects, and all of them drain your bank account.
If a provider’s treatment doesn’t pass a “common sense test,” and especially if they don’t physically examine you or don’t have the time to explain things in terms you understand, look elsewhere for your care.
What are some of the most recent advancements in the treatment of pain?
The three most promising areas in Pain Management are the advances being made in neuromodulation (spinal cord stimulators), genetically targeted medications, and advances in peripheral nerve radiofrequency ablation.
Neuromodulation uses electrical impulses to change the nerve signals from areas generating pain before they reach the brain. These are implanted devices that are similar to pacemakers, but instead of changing the heart rhythm they change the pain signals. These do really well for patients with chronic pain in their arms or legs.
 We have learned a lot about how our bodies process medication, and companies are now making genetically targeted medications that are specifically targeted to how individuals metabolize different drugs. In the future you will not have as much trial and error with medications. You will take a blood test, which will show which designer medication will work the best for you.
We have learned a lot about how our bodies process medication, and companies are now making genetically targeted medications that are specifically targeted to how individuals metabolize different drugs. In the future you will not have as much trial and error with medications. You will take a blood test, which will show which designer medication will work the best for you.
Radiofrequency ablation is an old technique where we use electrical energy to create heat, most often to drastically reduce pain along the spine itself. This technique is great in that, unlike most medications that reduce pain for a few hours, this works for six months or more. I have been using this successfully for years to help patients with low back and neck pain, but recent advances in the technology are allowing this to be used in other areas of the body as well. Knee and shoulder pain patients who have wanted to put off a replacement or were told by their orthopedic surgeon that they were not a good candidate can now achieve substantial long-lasting relief with radiofrequency ablation.
What kind of specialized training do pain management physicians have that my general or primary care physician might not have?
Pain Medicine is a subspecialty. It requires four years of medical school, four years of residency, and then a year of fellowship in an Accreditation Council for Graduate Medical Education approved program (this is all after grade school, high school and college, and thus requires 25 years of school/training at a minimum). During this training, pain management physicians learn how to safely and accurately perform a number of pain relieving procedures, extensive instruction in the use of medications, and exposure to a plethora of adjuvant modalities.
Any real Pain Management physician according to the American Board of Medical Specialties should have Board Certification first in one of four specialties (Anesthesiology, Physical Medicine and Rehabilitation, Psychiatry or Neurology), plus an additional Board Certification in Pain Medicine.
Unfortunately, Pain Management has one of the highest rates of non-trained imposters of any field in medicine. For some reason, physicians in multiple specialties often claim they do Pain Management, but they do not have the real training or they stopped short from going all the way through a Pain Medicine fellowship.
I don’t perform C-sections, even though I did 30 or so during my medical school/internship training because I know I don’t have the full training to do it safely. If you need a C-section, go to an OB-GYN. For some reason, that same, simple logic doesn’t seem to sink in with some physicians or some patients when it comes to pain management. Some seem to think, “Since the DEA says I can write for opioids, then I must be trained well enough to do chronic pain management.” This is not true. There are even online companies popping up selling “board certifications” from fake boards to help fraudulent providers trick patients. (These are like the internet ordinations for fake ministers.)
This is a definite “buyer beware” situation because some people are pedaling medications that are addictive and can be deadly if prescribed or used improperly. Same thing goes with doing injections. Just because you played an interventional pain doctor on TV, or stayed at a Holiday Inn last night, doesn’t mean you can safely place a needle inside the spinal canal without injuring the spinal cord. I hope patients spend a little time to make sure they are going to a reputable physician with all the proper training.
Our thanks to Dr. Solomon Pearce at the Mercy Pain Center for taking the time to answer our questions. Dr. Pearce is Double Board Certified in Pain Medicine and Physical Medicine and Rehabilitation. Before coming to Arkansas, Dr. Pearce was a Naval Flight Surgeon who served in multiple overseas deployments. For more information or to schedule a consultation with Dr. Pearce or his colleague Dr. Green at the Mercy Pain Center, call (479) 986-6199 or click HERE for more clinic info.